Iatrogenic edema of the arm
Iatrogenic lymphedema of the arm is lymphedema of the arm caused by treatment for a disease (such as breast cancer) or by previous surgery.
Diagnostic
- Lymphatic MRI is the test of choice for determining the indication for surgery, new lymph vessels, transplanted lymph nodes, and changes in lymph vessel growth.
- The results observed by isotopic lymphangiography show the absorption of the contrast fluid but, compared to the lymphatic MRI, they give little information on the rest of the network
Surgical Treatment
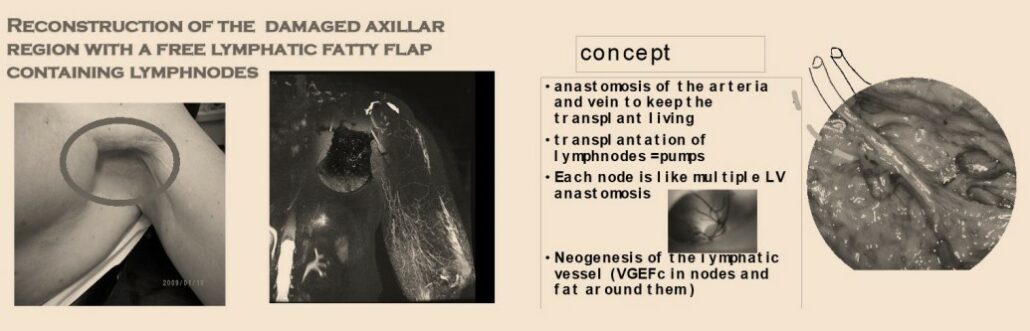
Lymph Nodes Transfer (LNT)
Autologous Lymph Nodes Transfer (ALNT), also called microsurgical vascularized lymph nodes transfer (VLNT) involves transferring a few healthy lymph nodes from one site to the affected area to restore the lymphatic function in the limb.
ALNT has many advantages. Check out who is a good candidate. All details about ALNT and iatrogenic arm lymphedema are here below.
- 40% final standardization
- 98% improvement
- 2% without result
- No worsening of lymphoedema
Results

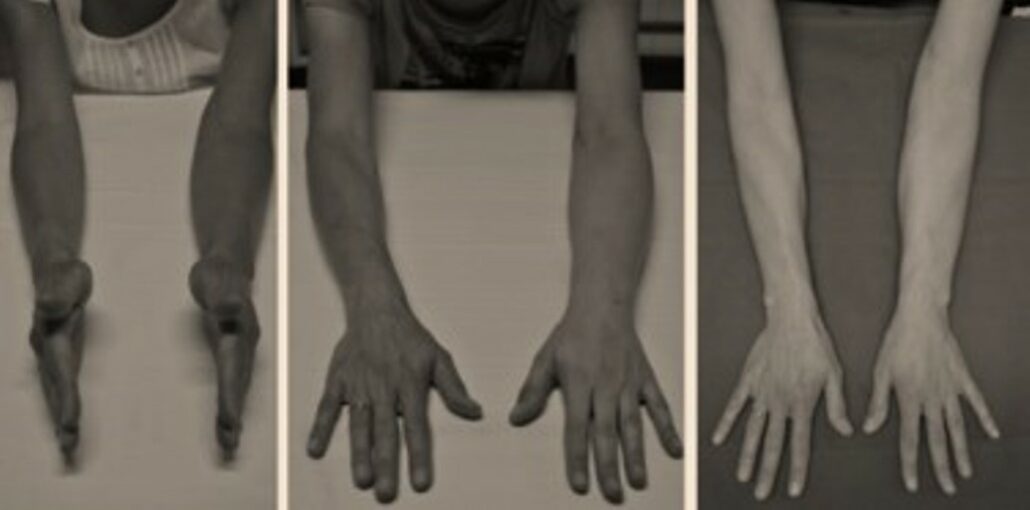
- Elephantiasis over 20 years old, with chronic infections, can be improved (as in this case, 4 years after LNT)
- Significant improvement in all cases but never complete recovery
- 98% improvement, but never complete normalization
- Decrease in infections
Moderate lymphedema
- Can be healed simply by adding certain knots like here.
- Scarring can be observed in these cases in 70% and improvement in all cases. The results will be stable after 1 year.
Lymphedema stage 2 and 3 (more advanced)
• Can be cured, but the combination with liposculpture to remove fatty deposits is important. It can be made the same assignment or later. The results will be better if the fibrous tissue is not too thick. operated as soon as possible, when the lymphoMRI shows no drainage. The normalization will be 40% of the cases, and the others will be improved by more than 50%
Lymphoedema stage 4
- Can be cured also in some cases, but it becomes difficult and 2 flaps can be mandatory plus liposculpture or local excisions must be combined
Effect on infections
- Decrease in chronic infections in 90% of cases
- Complete disappearance in 68% of cases
Effect on pain
- The pain that appears after an adenomectomy can be eliminated after surgery if the neuromas are treated.
- Pain and decreased tenderness in plexopathies may be improved, but improvement depends on damage to the plexus. Progressive degeneration of the nerves is stopped, but never really resolved
- Tendon transfer may be performed later to restore some functionality to the arm in cases of partial paralysis of the arm and hand.
Potential complications
The donor site does NOT create lymphedema if the dissection is well done.
The flap is NOT inguinal, but UPPER the inguinal fold and the 3.4 nodes removed are the lumbar area nodes and NOT THE LEG. But the anatomy should be well known and the surgeon should have good experience with this flap (and this flap has been known for 40 years for hand reconstruction – mac gregor flap). Injecting fluorescein into the feet can help prevent the lymph nodes draining from the leg from being removed.
- Seromas at donor sites reduced by restraints
- Slight temporary edema at the donor site (0.001%)
- Infections in 1% of cases
- Flap necrosis 2%
Lymphovenous anastomosis
The indications are limited to the early stages of the disease, when there is no fibrosis or sclerosis of the remaining lymphatic vessels, and life-long bandages are prescribed. The identification of good lymphatic vessels and the quality of the anastomosis are critical. Maintaining compression is essential to ensure high pressure in the lymphatic system. Many failures have therefore been reported with this technique.